

What are the differences in physiology in intubating children? There is a small cricothyroid membrane so landmarks for surgical airways are more difficult to locate.Young children have higher and more anterior tracheal openings than adults (C1 in infants, C7 in adults), therefore visualisation of the glottis is difficult.Large occiputs – neck flexed causes obstruction.Soft structures are at higher risk of airway trauma with repeated attempts causing oedema and further airway narrowing.Short trachea (high risk of endobronchial intubation).Think of Macroglossia seen in conditions such as Trisomy 21 and Beckwith-Wiedemann syndrome Larger tongue and adenoids – increases the difficulty in advancing the laryngoscope and visualizing the cords on laryngoscopy.Also, external compression can lead to rapid increase in airway resistance The airways are smaller! This might sound very obvious, however, this means that there is a lot less room for other things such as secretions, oedema and foreign bodies.Remember – you can intubate with a larger blade, but not a smaller one! If in doubt go for the bigger one!Īnatomical differences in paediatric vs adult airways

Royal Children’s Hospital Melbourne Airway Recommendations Please see your local policy for what is available in the area in which you work.
RAPID SEQUENCE INTUBATION PROCESS MAC
Miller are used in this age group due to their large floppy epiglottis and laxity of the ligament.ġ year MAC size 2 and 3 (size 3 usually 5 years upwards) Miller blades are better for neonates and young infants – up to 1 year then MAC blades are better.

MAC blades are curved to sit in the vallecula to lift the epiglottis indirectly but putting pressure on the glossoepiglottic ligament. Miller blades are straight blades which are designed to directly lift the epiglottis Bag valve mask with PEEP valve, oxygen on.Suction – large bore suction (x2 if soiled airway) under the pillow and turned on Have you considered calling for help? The definition of help will depend on your setting but could include Emergency Consultant, Anaesthetics or ICU.Įquipment required – remember the mnemonic SOAP ME
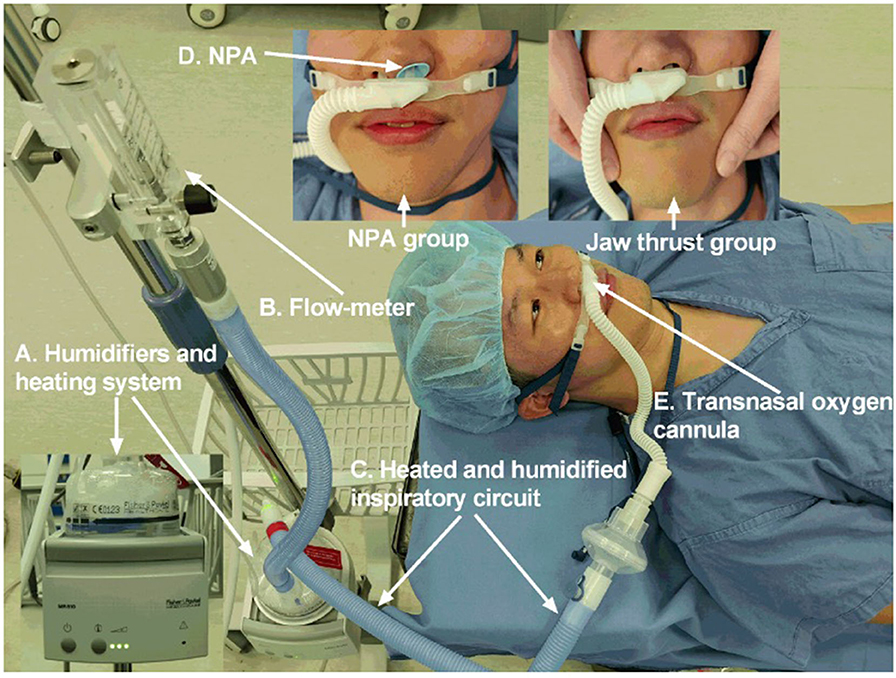
Labels on the front of scrubs can help the team know who is responsible for each role. This is the minimum set up – you may have more but ensure your roles are clearly allocated Procedure doctor – usually the drug giver Please check your hospital for your airway checklist – if you don’t have one, then check the ECI website for a blank version to create your own! They are a great aide memoire for a safe intubation. This is an example airway checklist from Liverpool Hospital, Sydney ( Airway Checklist) recommended by the Emergency Care Institute in Australia. This is a checklist to ensure that all aspects of the RSI have been thought about to mitigate any omissions during the procedure. However, oxygen demand and safe apnea times are very dependent on pulse rate, pulmonary function, red blood cell count, and numerous other metabolic factors.To ensure you are correctly prepared, we would advocate the use of an airway checklist. Other patients are given sedating and paralytic drugs to minimize discomfort. Even in apneic patients, such preoxygenation has been shown to improve arterial oxygen saturation and prolong the period of safe apneic time ( 2 General references Pulseless and apneic or severely obtunded patients can (and should) be intubated without pharmacologic assistance. Noninvasive ventilation (NIV) or high-flow nasal cannula (HFNC) can be used to aid preoxygenation ( 1 General references Pulseless and apneic or severely obtunded patients can (and should) be intubated without pharmacologic assistance. If time permits, patients should be placed on 100% oxygen for 3 to 5 minutes this measure may maintain satisfactory oxygenation in previously healthy patients for up to 8 minutes.


 0 kommentar(er)
0 kommentar(er)
